Rheumatoid Arthritis Case Study: Impact & Treatment
Question
Task: Complete the topic associated with the first letter of your Surname
A-G: Influenza B
H-M: Deep Vein Thrombosis
N-R: Rheumatoid Arthritis
S-Z: Shingles (Herpes Zoster)
In regards to your allocated topic, prepare a short fact sheet addressing the following questions:
1) Introduction and overview of the topic to include a definition, Australian incidence data (who is effected, how many) and known risk factors (age, gender, ethnicity etc). [300 words]
2) Describe pathophysiology of disorder with an in-depth discussion of underlying immunological mechanisms. How do these events alter normal homeostatic processes? [550 words]
3) Describe the pharmacological treatments detailing how the medications alter the underlying disease process (ie less focus on dosages and regimes and more focus on describing what the drug does and how that resolves the pathophysiology). If appropriate, include vaccinations. [ 250 words]
4) What are the key patient education considerations when nursing a patient with this disorder? (Bullet points) [250 words]
5) Conclusion [50 words]
*Extra 100 words not included in suggested word count above will allow for refs and expansion in other areas as you see fit.
Answer
Introduction
The concerned Rheumatoid Arthritis case study sheds light on an autoimmune disease, Rheumatoid Arthritis, in which cell of the immune system destroys residing tissue of bone. The disease is manifested by means of inflammation of joints, leading to pain and dysfunction of joints (Harrison et al., 2019). It is described in this Rheumatoid Arthritis case study that this disease mostly impacts the joints of both hands in the same period of time. The presence of a synovial membrane on the lining of the joint of the bones provides lubricant and minimise the friction. However, as the immune system attack the joint cells it weakens the synovial membrane leading to damage and erosion of bone.
According to the research conducted on this Rheumatoid Arthritis case study, in 2017-2019, 1.9% of the population of Australia was reported with Rheumatoid Arthritis that estimated to be 458,000 people (Australian Institute of Health and Welfare, 2019). According to the report of a National Health Survey, 13,213 hospitalisations have been documented in the year 2016-2017(Australian Institute of Health and Welfare, 2019). It was report that older adult of 70 year and above are the most affected group of population in Australia with Rheumatoid Arthritis. According to the report of AIHW considered in the context of Rheumatoid Arthritis case study, in the year 2017-2018, 5 % of the population belonging to age 55 to 65 years were reported with Rheumatoid Arthritis, whereas 8% of people of age 75 years were hospitalized due to Rheumatoid Arthritis (Australian Institute of Health and Welfare, 2020). It is evident from the research that the incidence of the disease is more common in female than male as there has been a report of 2.3% of women with Rheumatoid Arthritis compared with only 1.5% of men. In support of the above finding obtained in this Rheumatoid Arthritis case study, Australian Institute of Health and Welfare (2020) stated that 5 out of 8 women in Australia are having rheumatoid arthritis.
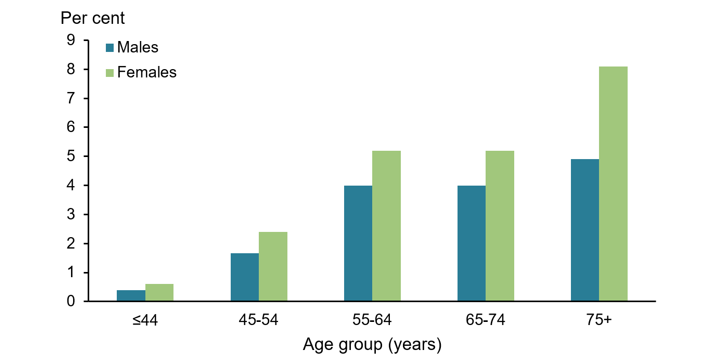
Figure 1: Incidence of Rheumatoid Arthritis by Age and Sex.
Source: (Australian Institute of Health and Welfare, 2019).
According to the report of Australian Institute of Health and Welfare (2018), it is stated herein Rheumatoid Arthritis case study that the pervasiveness of Rheumatoid Arthritis in the ethnic minority community was 2.3% as compared with 1.5% in the least disadvantage area due to the lack of access to medical health care and service and poor dietary management. However, it was mentioned that the data was not statistically significant.
Pathophysiology of Rheumatoid Arthritis
It is stated herein Rheumatoid Arthritis case study that the pathophysiology of the Rheumatoid Arthritis is an area of research to elucidate the role of aetiologic agents. In Rheumatoid Arthritis inflammation of the joint is the common noted occurrence that is initiated with the influx of the B cells, CD8+ and CD4+T Cells into the tissue membrane known as synovium (Guo et al., 2018). When the ailment is triggered, the immune cell of the body migrates to the joint and result in the formation of the cytokines and chemokines that activate and recruit other immune cells, for example, the CD4+. It is reported that CD4+ is recognise as an antigen by the antigen-presenting cells of the joint that stimulate macrophages and B cells and produce IL1 and TNF-? that release self-reactive antibodies in the synovium (Guo et al., 2018). Such a mediator is known to activate matrix-degrading enzyme causing destruction of bone. According to the research of Sokolove (2018) due to the accumulation of leukocyte and inundation of pro-inflammatory mediator tends to form inflammatory cascade that is characterised through fibroblast-like synoviocytes (FLS) by means of dendritic cells, B cell, T cells and monocyte.
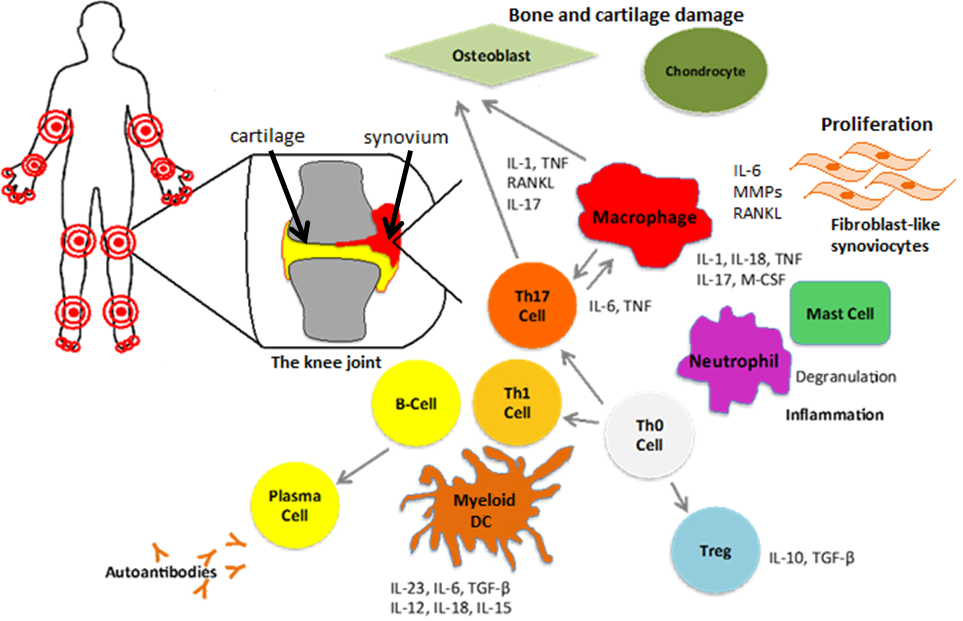
Figure 2: Pathophysiology of Rheumatoid Arthritis
Source: (Guo et al., 2018)
The cell-mediated and humoral immunity are progressively involved in the formation of ACPA that causes chronic synovitis. The monocyte and macrophage have been reported to enormously permeate the synovial membrane which is central to the occurrence of inflammation and swelling. The immune cells are then intimately indulged in the formation of anti-citrullinated protein antibodies (ACPA) causing inflammation of the bone. In support of this finding Derksen et al. (2017) stated that expression of FOXO3a transcription factor of immune cells gets increases as with the aggregation of T cells in increasing the survival of these cells in the synovial tissue contributing in chronic inflammation. It is also noted herein Rheumatoid Arthritis case study that ACPA increases the activity of NF-Kb and TNF-? with binding Grp-78 due to which ?-Enolase induces the secretion of M1 Macrophage and M2 macrophage (Guo et al., 2018). Research has indicated that due to the imbalance of M1/M2 monocytes, osteoclastogenesis takes place (Venuturupalli, 2017).
Research has indicated that due to the inflammatory cascade, stimulate FLS and cause a release of metalloprotease that disassemble and degrade the type II collagen of cartilage. Conversely, the production of IL1 and 17A cytokines and reactive oxygen and nitrogen, the chondrocytes present in cartilage undergo apoptosis (McInnes et al., 2016). The erosion of bone has remained a controversial topic between inflammation and autoimmunity in rheumatoid arthritis. The loss of bone is manifested as the induction and suppression of osteoclast and osteoblast. Research says that due to the secretion of IL-6, IL7, IL-1? and TNF-?, are known to cause pro-osteoclastogenic impact and that suppress the formation of bone due to the signal from RANKL (receptor activator of nuclear factor kappa-B ligand) and M-CSF (macrophage colony-stimulating factor) (Nerurkar et al., 2019). The influence of such a signal can be seen by the augmented influx and division of the monocyte cells into osteoclast in the light of inflammation. Similarly, another mechanism suggests that against the citrullinated proteins, anti-citrullinated antibodies are formed that make the osteoclast vulnerable target for the self-antibody. In the research of Weitzmann and Ofotokun (2016), it is noted that ACPA tends to bind with the osteoclast that causes loss of bone cells and destruction of subchondral bone. As the impact of such changes, the degeneration of the articular cartilage is noted thus disrupting the normal homeostatic process.
What is the role of Pharmacological treatment in the scenario of Rheumatoid Arthritis case study? Explain.
With the identification of the preclinical stage and the pathophysiology of rheumatoid arthritis, the development of new potential pharmacological intervention has taken place. The leflunomide is the potent drug that is effective in reducing the inflammation of the joint as they interact with the dihydroorotate enzyme and inhibit its action which is critical for replication of DNA and RNA of the leukocyte (Guo et al., 2018). Thus, with the intake of the drug, the T cell infiltration is stopped and inhibits tyrosine kinase which is secondary for the T cell and B cell signalling. Similarly, Sulfasalazine drug reduces the active joints counts by the action of its two metabolites sulfapyridine and 5-aminosalicylic acid. Research suggests that Sulfasalazine at the location of inflammation increases the formation of adenosine which is effective in inhibiting the formation of osteoclast via modulatory impact on RANKL (Ford et al., 2018). This, in turn, causes apoptosis of macrophage resulting in inhibition of TNF-? and suppression of B cell. Thus, the secretion of self-antibody is stopped and erosion of bone does not take place.
Another most potent drug known as hydroxychloroquine is been used as the mean of treatment of rheumatoid arthritis. Research by Schrezenmeier and Dörner (2020) outlined in this Rheumatoid Arthritis case study suggests that the drugs are designated to involve in the action of T cell and Antigen-presenting cells (macrophage) which are responsible for inflammation of joints. The drug is effective in reducing the secretion of pro-inflammatory cytokines and TNF, as its impact can be seen in the lowering the production of the protease enzyme by the synovium and normalising the inflammation of bone joints.
Patient education
Education and counselling are crucial nursing interventions that assist the patient in understanding the disease process of Rheumatoid Arthritis and cope with the underlying challenges (Metwaly et al., 2017). Some of the key patient education consideration given by the nurse for effective management of Rheumatoid Arthritis is as follows:
- Education about disease process: The nurses are required to provide knowledge about the disease process and the associated symptoms to make the patient mindful about their disease as it can make the patient involve in its management process.
- Medication information: It is noted in the research on Rheumatoid Arthritis case study that medication for Rheumatoid Arthritis needs to be taken in the correct dose as side effects are prevalent if exploited (Smolen et al., 2017). Therefore, the nurse should give education about the importance of dose size and administration of medicine in time. Additionally, the nurse should make the patient aware of the potential side effect of the drugs like dizziness, nausea and advise them to contact their GP immediately in case of the occurrence of such signs.
- Exercise regime: The words of Metwaly et al. (2017) explored in this segment of Rheumatoid Arthritis case study have noted that for effective management of disease, medication therapy must be combined with the physical exercise as it can be useful in relieving pain and stiffness. Therefore, the patient must be educated about the need for physical exercise or occupational therapy and suggest them to visit the physical therapist.
- Coping with daily living activities: Rheumatoid Arthritis patients may feel energy depleted; it is crucial to teach them to the method to pace themselves and way to prioritise their daily activities to make them unable to achieve their daily living goal.
- Educating for joint protection: In rheumatoid arthritis, other bone also becomes vulnerable to damage if safety measures are not taken. Therefore, the nurse should educate the patient for a different way of projecting the joint like opening the door slowly and not lifting heavy materials.
Conclusion
Lastly, the above Rheumatoid Arthritis case study concludes by saying that Rheumatoid Arthritis is lethal bone disorder and its prevalence and burden can increase any appropriate measure that is not taken by the people. As exemplified in this brief review of Rheumatoid Arthritis case study, the pathophysiology of Rheumatoid Arthritis can help to provide a new therapeutic approach for its management. However, the government should take initiative for its proper management, particularly for the people living in remote areas so that the burden of disease could be lowered.
Reference
Australian Institute of Health and Welfare. (2018). Rheumatoid arthritis, Impact of Rheumatoid Arthritis - Australian Institute of Health and Welfare. Retrieved 3 April 2020, from https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/rheumatoid-arthritis/contents/who-gets-rheumatoid-arthritis
Australian Institute of Health and Welfare. (2019). Report and data of Rheumatoid arthritis. Aihw.gov.au. Rheumatoid Arthritis case study Retrieved 3 April 2020, from https://www.aihw.gov.au/getmedia/1e295637-e5fb-4059-a1d8-eb3936cfa7a9/phe188-rheumatoid-arthritis-factsheet.pdf.aspx?inline=true.
Australian Institute of Health and Welfare. (2020). Rheumatoid arthritis, what is rheumatoid arthritis? - Australian Institute of Health and Welfare. Australian Institute of Health and Welfare. Retrieved 3 April 2020, from https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/rheumatoid-arthritis/contents/what-is-rheumatoid-arthritis.
Derksen, V. F. A. M., Huizinga, T. W. J., & van der Woude, D. (2017, June). The role of autoantibodies in the pathophysiology of rheumatoid arthritis. In Seminars in immunopathology (Vol. 39, No. 4, pp. 437-446). Springer Berlin Heidelberg. https://doi.org/10.1007/s00281-017-0627-z
Ford, M., Sahbudin, I., Filer, A., Steven, N., & Fisher, B. A. (2018). High proportion of drug hypersensitivity reactions to sulfasalazine following its use in anti-PD-1-associated inflammatory arthritis. Rheumatology, 57(12), 2244-2246. https://doi.org/10.1093/rheumatology/key234
Guo, Q., Wang, Y., Xu, D., Nossent, J., Pavlos, N. J., & Xu, J. (2018). Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies. Bone research, 6(1), 1-14. https://dx.doi.org/10.1038%2Fs41413-018-0016-9
Harrison, S. R., Li, D., Jeffery, L. E., Raza, K., & Hewison, M. (2019). Vitamin D, autoimmune disease and rheumatoid arthritis. Rheumatoid Arthritis case study Calcified tissue international, 1-18. https://doi.org/10.1007/s00223-019-00577-2
McInnes, I. B., Buckley, C. D., & Isaacs, J. D. (2016). Cytokines in rheumatoid arthritis—shaping the immunological landscape. Nature Reviews Rheumatology, 12(1), 63. https://doi.org/10.1038/nrrheum.2015.171
Metwaly, E. A., Taha, N. M., Seliem, H. A. E. W., & Sakr, M. D. (2017). Effectiveness of non-pharmacological nursing intervention program on female patients with rheumatoid arthritis. Central European Journal of Nursing and Midwifery, 8(3), 682-690. DOI: 10.15452/CEJNM.2017.08.0019
Nerurkar, L., Siebert, S., McInnes, I. B., & Cavanagh, J. (2019). Rheumatoid Arthritis and depression: an inflammatory perspective. The Lancet Psychiatry, 6(2), 164-173. https://doi.org/10.1016/S2215-0366(18)30255-4
Schrezenmeier, E., & Dörner, T. (2020). Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Nature Reviews Rheumatology, 1-12. https://doi.org/10.1038/s41584-020-0372-x
Smolen, J. S., Landewé, R., Bijlsma, J., Burmester, G., Chatzidionysiou, K., Dougados, M., ... & Aletaha, D. (2017). EULAR recommendations for the management of Rheumatoid Arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Annals of the rheumatic diseases, 76(6), 960-977. http://dx.doi.org/10.1136/annrheumdis-2016-210715
Sokolove, J. (2018). Rheumatoid Arthritis pathogenesis and pathophysiology. In Lung Disease in Rheumatoid Arthritis (pp. 19-30). Rheumatoid Arthritis case study Humana Press, Cham. https://doi.org/10.1007/978-3-319-68888-6_2
Venuturupalli, S. (2017). Immune mechanisms and novel targets in rheumatoid arthritis. Immunology and Allergy Clinics, 37(2), 301-313. https://doi.org/10.1016/j.iac.2017.01.002
Weitzmann, M. N., & Ofotokun, I. (2016). Physiological and pathophysiological bone turnover—role of the immune system. Nature Reviews Endocrinology, 12(9), 518. https://doi.org/10.1038/nrendo.2016.91












